ADHD Sleep Tips & Bedtime Routine
If bedtime at your house feels like a nightly battle, you're not alone. Sleep challenges are one of the most common struggles for families with ADHD children, and honestly, it makes perfect sense when you understand how ADHD affects the brain.
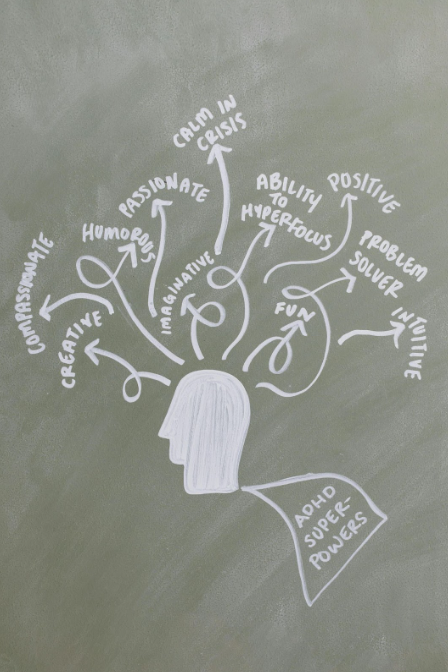
The same neurological differences that make your child energetic, creative, and wonderfully unique during the day can make winding down at night feel nearly impossible. But here's what I want you to know: sleep problems aren't a character flaw or a parenting failure. They're a real symptom of ADHD that deserves the same attention and strategy as any other challenge your child faces.
After working with hundreds of families over the years, I've seen how the right approach to sleep can transform not just bedtime, but your child's entire day. Better sleep means better focus, improved emotional regulation, and a calmer household for everyone.
Why ADHD Makes Sleep So Hard
Understanding the "why" behind sleep struggles helps you approach them with more patience and better strategies. ADHD affects sleep in several key ways:
The Brain Won't "Turn Off"
ADHD brains have difficulty with what researchers call "cognitive arousal." While your child's body might be tired, their mind is still racing with thoughts, ideas, worries, or excitement about tomorrow. It's like trying to fall asleep while someone's playing loud music in your head. Research shows that people with ADHD traits consistently report poorer sleep, and between 70–90% of individuals with ADHD experience significant sleep problems. In two separate studies, scientists found that ADHD symptoms were strongly linked with both cognitive and physical pre-sleep arousal, but it was cognitive arousal that most reliably explained insomnia severity. In fact, in one dataset, 80% of the effect of ADHD symptoms on sleep difficulties was driven by racing thoughts before bed.
Melatonin Production Issues
Many children with ADHD have delayed melatonin production. Melatonin is the hormone that makes us feel sleepy, and for kids with ADHD, it often doesn't kick in until much later than it should. This isn't laziness or stalling - it's biology.
Hyperactivity Doesn't Have an Off Switch
That physical energy that keeps your child moving all day doesn't magically disappear at 8 PM. Their body may still feel wired even when they're exhausted.
Anxiety and Racing Thoughts
Nighttime is often when worries surface. Without the distractions of daytime activities, children with ADHD may find themselves thinking about everything that happened today or everything that might happen tomorrow.
The Foundation: Sleep Environment That Works
Before we talk routines, let's set up your child's room for sleep success.
Make It Cool and Dark
ADHD brains are often overstimulated, so create a sensory-friendly sleep environment:
Keep the room between 65-68 degrees
Use blackout curtains or an eye mask
Consider a white noise machine to block out household sounds
Remove or cover any LED lights from electronics
Address Sensory Needs
Many children with ADHD have sensory processing differences that affect sleep:
Weighted blankets can provide calming deep pressure
Soft, breathable pajamas without tags or rough seams
Comfortable pillows - some kids need extra firm, others prefer soft
Consider letting them sleep with a favorite stuffed animal or blanket for comfort
Create a Tech-Free Zone
The blue light from screens interferes with melatonin production, which is already challenging for ADHD brains. Make bedrooms a screen-free space at least an hour before sleep time.
Building an ADHD-Friendly Bedtime Routine
The key to bedtime success is starting your routine much earlier than you might think. For most ADHD children, the bedtime routine should begin 60-90 minutes before you want them actually asleep.
Phase 1: The Wind-Down Begins (90 minutes before sleep)
Start shifting the energy in your entire house:
Dim the lights throughout your home
Turn off exciting TV shows or video games
Begin speaking in quieter voices
Reduce household activity and noise
Phase 2: Physical Preparation (60 minutes before sleep)
This is when the actual bedtime routine begins:
Light snack if your child is hungry (hunger can keep them awake)
Warm bath or shower - the drop in body temperature afterward naturally triggers sleepiness
Put on comfortable pajamas
Use the bathroom - make this non-negotiable to avoid middle-of-the-night trips
Phase 3: Calming Activities (30-45 minutes before sleep)
Choose quiet, soothing activities that help the brain transition:
Reading together (you read to them, or they read quietly)
Gentle stretching or simple yoga poses
Listening to calm music or nature sounds
Drawing or coloring
Simple breathing exercises or progressive muscle relaxation
Avoid: exciting books, stimulating conversations about tomorrow's plans, or anything that might rev up their brain again.
Phase 4: Connection and Comfort (15-30 minutes before sleep)
This is often the most important part for children with ADHD:
Quiet conversation about the day - focus on positive moments
Physical affection - cuddling, back rubs, or gentle massage
Reassurance about any worries or concerns
Consistent goodnight routine - same words, same actions, same comfort items
Specific Strategies for Common ADHD Sleep Challenges
"My child says they're not tired"
This is often true! Their melatonin may not have kicked in yet. Instead of arguing, try:
Saying "Your body needs rest even if your brain doesn't feel tired"
Allowing quiet activities in bed like audiobooks or soft music
Using a visual timer so they know how long "quiet time" will last
Implementing "bedroom time" rather than demanding immediate sleep
"They keep getting up for water, bathroom, one more hug"
Set clear expectations during the day:
Address all needs before the final goodnight - bathroom, water, snacks, comfort items
Create a bedtime pass system - give them one ticket they can use for one out-of-bed request
Stay calm and consistent - walk them back to bed without long conversations
Consider if they have legitimate needs - some children do need a small snack or extra reassurance
"Their mind races with worries or excitement"
Help them process thoughts before bedtime:
Keep a worry journal by their bed - write down concerns to deal with tomorrow
Practice gratitude - name three good things from the day
Use guided meditation or relaxation apps designed for children
Talk through tomorrow's plan earlier in the evening, not right before sleep
"They wake up multiple times during the night"
Night wakings are common with ADHD:
Keep their room completely dark - even small lights can wake ADHD brains
Teach them what to do if they wake up - stay in bed, use relaxation techniques, listen to quiet music
Avoid bringing them to your bed unless it's truly necessary - it creates habits that are hard to break
Consider if medication timing might be affecting sleep (discuss with your doctor)
The Role of Daytime Activities in Better Sleep
What happens during the day dramatically affects nighttime sleep for children with ADHD.
Physical Activity is Crucial
ADHD children need significant physical activity during the day to sleep well at night:
Aim for at least 60 minutes of moderate to vigorous exercise
Outdoor time is especially beneficial - natural light helps regulate circadian rhythms
Avoid intense physical activity within 2-3 hours of bedtime
Manage Afternoon and Evening Stimulation
Limit caffeine (including chocolate) after 2 PM
Be strategic about exciting activities - birthday parties, play dates, or high-energy games should end well before bedtime
Create calm transitions between high-energy and low-energy activities
Consider Nap Timing
For younger children who still nap:
No naps after 3 PM
Keep naps short (30-60 minutes max)
Some children may need to give up naps earlier than neurotypical peers to sleep well at night
When Sleep Medications Might Help
Sometimes behavioral strategies aren't enough, and that's okay. Many children with ADHD benefit from melatonin supplementation or other sleep aids.
Melatonin: The Basics
Start with the lowest dose possible (usually 0.5-1 mg)
Give it 30-60 minutes before desired sleep time
It works best when combined with good sleep hygiene, not as a standalone solution
Talk to your child's doctor before starting any medication
Other Considerations
Some ADHD medications can interfere with sleep - discuss timing with your doctor
Anxiety medications might be helpful if worry is the main sleep disruptor
Always work with a healthcare provider who understands ADHD
Creating Consistency Across Different Environments
Your child needs good sleep whether they're at home, at a relative's house, or even in a hotel room.
Portable Sleep Kit
Create a bag with:
Favorite stuffed animal or blanket
White noise app on a phone or tablet
Familiar pajamas
Any comfort items that help with sleep
Communicate with Other Caregivers
Make sure grandparents, babysitters, or other family members understand:
Your child's specific bedtime routine
Which steps are non-negotiable vs. which can be flexible
How to handle common challenges that arise
Adjusting Expectations and Celebrating Progress
Here's the truth about ADHD and sleep: perfect nights may be rare, and that's normal. Instead of aiming for perfection, celebrate improvements:
Going to bed without a major meltdown
Staying in their room all night (even if they didn't sleep immediately)
Waking up less grumpy in the morning
Being able to follow more of the bedtime routine independently
Track What's Working
Keep a simple sleep log for a few weeks:
What time did bedtime routine start?
How long did it take to fall asleep?
Any middle-of-the-night wakings?
Morning mood and energy level
Look for patterns. Maybe your child sleeps better after particularly active days, or struggles more when they've had screen time close to bedtime.
Seasonal and Developmental Changes
Expect your child's sleep needs and patterns to change:
Seasonal Adjustments
Summer: Longer daylight can delay melatonin production
Winter: Less natural light might require earlier bedtimes or light therapy
School vs. vacation: Maintain some structure even during breaks
Growing and Changing Needs
Sleep needs decrease with age - a 6-year-old needs more sleep than a 12-year-old
Puberty brings major sleep changes - teenagers naturally shift to later bedtimes
Medication adjustments might affect sleep patterns
When to Seek Professional Help
Consider consulting a sleep specialist or your child's healthcare provider if:
Sleep problems persist despite consistent strategies for 4-6 weeks
Your child's daytime functioning is significantly impacted
The whole family's sleep is being disrupted regularly
You suspect sleep apnea, restless leg syndrome, or other sleep disorders
Red Flags That Need Immediate Attention
Loud snoring or breathing problems during sleep
Extremely restless sleep with constant movement
Sleepwalking or other unusual nighttime behaviors
Severe anxiety or panic attacks at bedtime
Your Sleep Success Plan
Ready to make changes? Here's how to start:
Choose one area to focus on first - maybe the bedtime routine or the sleep environment
Involve your child in the process - let them help create their ideal sleep space or routine
Be consistent for at least two weeks before making major adjustments
Track progress without obsessing over perfect nights
Celebrate small wins - every improvement matters
Remember, establishing healthy sleep patterns takes time, especially for children with ADHD. Their brains are working differently, not defectively. With patience, consistency, and the right strategies, you can help your child develop the sleep skills they need to thrive.
Your child can learn to sleep well. It might take longer than you'd like, and the path might look different from other families, but better sleep is absolutely possible. You're not just helping them get through the night - you're giving them a foundation for better days, improved focus, and emotional regulation that will benefit them for years to come.
You’ve got this, one night at a time.